
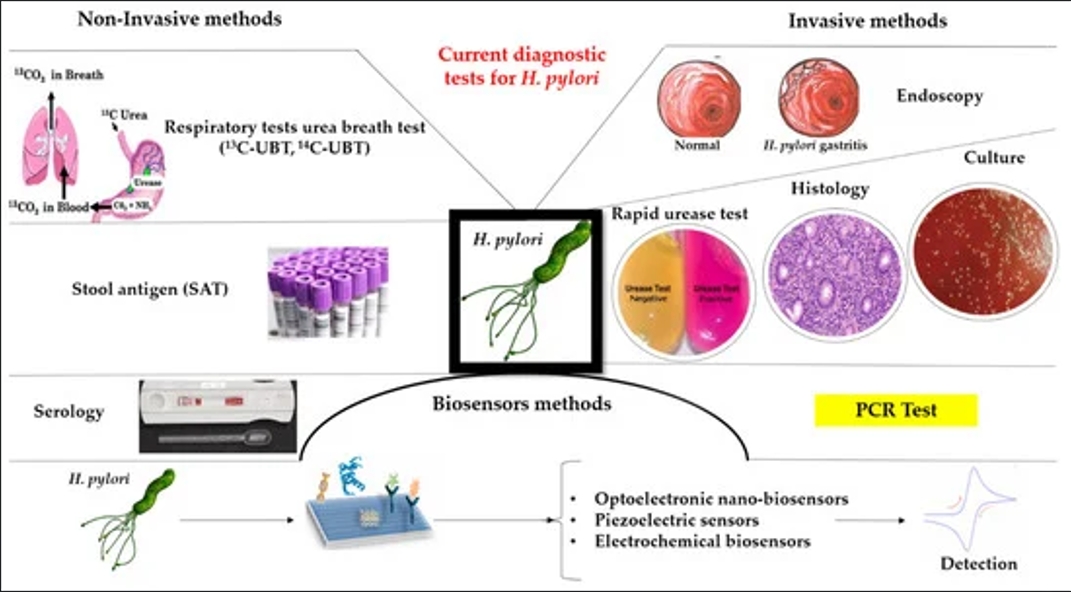
Helicobacter pylori (H. pylori) is a common pathogenic bacterium in the stomach, closely associated with gastritis, peptic ulcers, and gastric cancer. Accurate detection of H. pylori is crucial for diagnosis and treatment. Current clinical detection methods can be classified as invasive and non-invasive, each with its own advantages and limitations. This article provides a detailed comparison of these methods and evaluates their accuracy.
I. Invasive Detection Methods
1. Endoscopy with Rapid Urease Test (RUT)
Principle: A gastric mucosal biopsy is obtained during endoscopy. H. pylori produces urease, which breaks down urea into ammonia and CO₂, raising the pH and causing a color change in a pH-sensitive indicator.
Advantages:
✅Fast and simple (results in 30 minutes to a few hours)
✅Relatively low cost
✅High specificity (90–95%)
Disadvantages:
✅Sensitivity depends on biopsy location (80–90%)
✅Requires endoscopy, causing patient discomfort
✅False negatives possible if the patient recently used antibiotics, proton pump inhibitors (PPIs), or has gastric bleeding
2. Histological Examination
Principle: Biopsy samples are stained (e.g., hematoxylin-eosin, Giemsa, or immunohistochemical staining) and examined under a microscope for bacterial presence.
Advantages:
✅Direct visualization of bacteria and gastric mucosal damage
✅Near 100% specificity
✅Can assess gastritis severity and atrophy
Disadvantages:
✅Depends on pathologist expertise
✅Higher cost and longer processing time
✅Sampling errors may lead to false negatives
3. Bacterial Culture
Principle: Gastric biopsy samples are cultured on specialized media to grow H. pylori.
Advantages:
✅100% specificity (gold standard)
✅Allows antibiotic susceptibility testing
✅Useful for research purposes
Disadvantages:
✅Lower sensitivity (70–80%)
✅Technically challenging, requiring strict culture conditions
✅Time-consuming (3–7 days for results)
✅Expensive
II. Non-Invasive Detection Methods
1. Urea Breath Test (UBT)
Principle: The patient ingests urea labeled with ¹³C or ¹⁴C. H. pylori urease breaks it down into labeled CO₂, which is detected in exhaled breath.
Advantages:
✅High accuracy (95% sensitivity, 95% specificity)
✅Non-invasive, well-tolerated
✅Reflects whole-stomach infection (no sampling bias)
✅Ideal for post-treatment monitoring
Disadvantages:
✅Requires stopping PPIs (2 weeks) and antibiotics (4 weeks) before testing
✅¹⁴C-UBT has minimal radioactivity (but considered safe)
✅¹³C-UBT is more expensive
2. Stool Antigen Test (SAT)
Principle: Detects H. pylori antigens in stool samples.
Advantages:
✅Non-invasive, suitable for children
✅Sensitivity 85–95%, specificity 90–95%
✅Useful for post-treatment evaluation
✅Rapid results with some kits
Disadvantages:
✅Results may be affected by stool consistency
✅Some patients dislike stool sampling
✅Monoclonal antibody tests are more expensive
3. Serological Testing
Principle: Measures IgG antibodies against H. pylori in blood.
Advantages:
✅Unaffected by recent medication use
✅Easy sample collection
✅Useful for epidemiological studies
Disadvantages:
✅Cannot distinguish active vs. past infection
✅Not suitable for post-treatment monitoring (antibodies persist for months/years)
✅Lower accuracy (80–90% sensitivity, 70–90% specificity)
III. Accuracy Comparison of Detection Methods
| Method | Sensitivity(%) | Specificit(%) | Advantages | Disadvantages |
| Rapid Urease Test (RUT) | 80-90 | 90–95 | Fast, low cost | Invasive, sampling errors |
| Test (RUT) Histology |
90–95 |
95–100 |
Assesses mucosal |
Pathologist-dependent, time-consuming |
| Bacterial Culture |
70–80 |
100 |
Gold standard, antibiotic testing |
Technically difficult, slow |
| Urea Breath Test (UBT) |
95 |
95 | Non-invasive, highly accurate |
Requires stopping medications |
| Stool Antigen Test (SAT) |
85–95 |
90–95 |
Non-invasive, good for children |
Sampling discomfort |
| Serology |
80-90 | 7-90 | Unaffected by medications |
Cannot confirm active infection |
IV. Clinical Recommendations
Most Accurate Method:
✅Urea Breath Test (UBT) is the most accurate non-invasive method, especially ¹³C-UBT (no radiation).
✅Bacterial culture is the gold standard but is impractical for routine use.
Method Selection by Scenario:
✅Initial diagnosis: UBT or SAT preferred; endoscopy + RUT/histology if mucosal assessment is needed.
✅Post-treatment follow-up: UBT or SAT (after 4 weeks off antibiotics).
✅Epidemiological studies: Serology or SAT.
✅Children: ¹³C-UBT or SAT.
✅Antibiotic resistance testing: Bacterial culture + susceptibility testing.
Important Considerations:
✅Stop PPIs for 2 weeks and antibiotics for 4 weeks before testing.
✅Active bleeding may reduce RUT/UBT accuracy.
✅Atrophic gastritis may lower UBT sensitivity.
Conclusion:
The choice of H. pylori detection method depends on accuracy, feasibility, patient factors, and clinical needs. UBT is the preferred choice due to its high accuracy and non-invasive nature, but multiple methods may be combined in certain cases.